

The Advantages Of A National Asbestos Law Firm
Access To Top Legal Talent Nationwide
When facing a mesothelioma diagnosis, the complexity of asbestos litigation demands specialized legal knowledge. National asbestos law firms bring together attorneys who focus solely on these types of cases. This concentration means they possess a deep familiarity with the specific laws, precedents, and tactics involved in asbestos claims. They have honed their skills through years of dedicated practice, often accumulating decades of collective experience. This specialized focus allows them to build stronger cases and pursue compensation more effectively than a general practice attorney might. Their nationwide reach also means they can draw upon a wider pool of legal talent, ensuring your case is handled by some of the most experienced lawyers in the field. Reviewing the range of practice areas covered by established personal injury firms can help victims understand whether a firm’s experience extends beyond asbestos to cover related claims like veterans’ benefits or disability.
Broader And Specialized Legal Experience
Mesothelioma cases often involve more than just the initial exposure. They can intersect with other legal areas, such as disability claims, veterans’ benefits, or even medical malpractice related to delayed diagnosis. A national asbestos law firm typically has attorneys with a broad range of experience, allowing them to address these related issues. This means they can look at your situation from multiple angles, identifying all potential avenues for compensation. They understand the intricacies of asbestos trust funds, for example, which can be a significant source of recovery for victims. This dual focus—specialized knowledge of asbestos law combined with broader legal capabilities—is vital for maximizing a client’s recovery.
Resources To Hold Corporations Accountable
Companies responsible for asbestos exposure often have substantial financial resources and experienced legal teams. To effectively challenge them, your legal representation needs comparable resources. National firms are structured to handle these large-scale corporate adversaries. They have the financial backing to cover extensive investigations, hire top medical and industry experts, and fund lengthy court battles if necessary. This financial strength is critical because it allows them to pursue claims without upfront costs to the client and to negotiate from a position of power. They are prepared to go to trial if a fair settlement cannot be reached, demonstrating a commitment to securing the best possible outcome for their clients. This ability to stand up to powerful corporations is a key advantage of working with a well-established national asbestos law firm like this one.
Why A Nationwide Presence Matters For Mesothelioma Justice
When facing a mesothelioma diagnosis, the location of your legal representation can make a significant difference in the outcome of your case. While a local attorney might seem convenient, a law firm with a nationwide reach brings distinct advantages that are particularly important for mesothelioma claims.
Ability To File Claims In All 50 States
Mesothelioma cases often involve complex exposure histories that may span multiple states or even decades. A firm that operates across the country isn’t limited to filing a claim in just one jurisdiction. They can strategically choose the state that offers the most favorable legal environment for your specific situation. This might mean:
- Filing where the statute of limitations provides more time.
- Pursuing claims in states with laws that better support asbestos victims.
- Bringing action against companies based in states where they have a significant presence.
This flexibility is key to maximizing your potential compensation. A national firm’s reach also means clients can access office locations across the country — reviewing asbestos law firm office locations nationwide is a practical starting point for patients identifying representation in their region.
Navigating Statute Of Limitations Across Jurisdictions
Every state has its own deadlines, known as statutes of limitations, for filing legal claims. These deadlines can be confusing and vary widely. A national law firm has the experience to track these different rules and ensure your claim is filed within the correct timeframe, no matter where the exposure occurred or where the responsible parties are located. Missing a deadline can mean losing your right to seek compensation entirely. They understand how to manage these varying timelines to keep your case on track.
Established Reputation With Manufacturers
Large corporations and asbestos manufacturers are aware of the law firms that consistently take them to court and win. A firm with a strong national reputation often commands respect from these companies. This established presence can lead to quicker settlements, as manufacturers may prefer to resolve cases with well-known, formidable legal teams rather than face them in a lengthy trial. This can mean faster access to the compensation you and your family need.
The Expertise Of A National Asbestos Law Firm
When facing a mesothelioma diagnosis, the legal path can seem complicated. This is where the specialized knowledge of a national asbestos law firm becomes important. These firms bring together attorneys who have dedicated their careers to asbestos litigation, giving them a deep well of knowledge.
Centuries Of Cumulative Legal Experience
Lawyers at national firms often have decades of experience, sometimes spanning over 45 years, focused solely on asbestos cases. This isn’t just general legal practice; it’s a specific focus on the unique challenges of mesothelioma claims. They’ve seen many cases, learned from them, and developed strategies that work. This extensive history means they understand the tactics asbestos companies might use to avoid paying compensation. Firms that also handle a broad range of personal injury practice areas can identify additional compensation avenues that a purely asbestos-focused firm might overlook.
Focus On Mesothelioma Litigation Nuances
Mesothelioma cases are not like other personal injury claims. They involve complex medical details, long latency periods between exposure and diagnosis, and specific legal hurdles. Attorneys at national firms concentrate on these nuances. They know how to connect past exposures, often decades ago, to a current diagnosis. This focus allows them to build stronger arguments and present them effectively in court or during settlement negotiations.
Understanding Asbestos Trust Funds
Many companies that produced or used asbestos have set up trust funds to compensate victims. These funds have specific rules and claim processes. A national asbestos law firm will be well-versed in:
- Identifying all relevant asbestos trust funds.
- Filing claims correctly and within the required timelines.
- Gathering the necessary medical and exposure evidence for each fund.
- Pursuing claims from multiple sources, including trusts and lawsuits, to maximize potential compensation.
How A National Firm Supports Your Case
Comprehensive Case Investigation
When you’re dealing with a serious illness like mesothelioma, the last thing you want to worry about is digging up old records or tracking down former coworkers. A national asbestos law firm takes on this burden for you. They have the resources to conduct a thorough investigation into your exposure history. This often involves:
- Reviewing company documents and product information.
- Identifying potential job sites and workplaces where asbestos exposure may have occurred.
- Interviewing former colleagues and witnesses who may recall exposure details.
This detailed groundwork is key to building a strong foundation for your claim. Patients ready to take the first step can also contact a personal injury legal team directly for an initial assessment of their exposure history and compensation eligibility.
Access To Medical And Industry Experts
Mesothelioma cases require specialized knowledge. National firms have established connections with a network of medical professionals and industry experts. These individuals can provide critical testimony and analysis, such as:
- Explaining the link between asbestos exposure and your specific diagnosis.
- Assessing the severity of your condition and its impact on your life.
- Providing insights into industry practices and corporate knowledge of asbestos risks.
Their input helps to clearly demonstrate the cause of your illness and the extent of the harm you have suffered.
Dedicated Trial Teams For Every Case
Filing a mesothelioma claim can be complex, and having a dedicated team in your corner makes a difference. National firms assemble specialized legal teams focused on asbestos litigation. This means your case is handled by attorneys and support staff who understand the unique aspects of these claims. They work to:
- Develop a tailored legal strategy for your situation.
- Manage all legal filings and deadlines efficiently.
- Prepare thoroughly for negotiations or, if necessary, trial.
Choosing The Right Legal Representation
Comparing National Firms To Local Options
When facing a mesothelioma diagnosis, selecting the right legal team is a significant decision. While local attorneys might seem like a convenient choice, national asbestos law firms often bring a distinct set of advantages to the table. These firms typically have a broader reach and more specialized experience, which can be particularly beneficial in complex cases involving asbestos exposure. They are equipped to handle claims across different states, a capability that can be vital given the varied laws and deadlines that apply from one jurisdiction to another. The firm you choose can directly impact the outcome and the compensation you receive.
The Importance Of Proven Results
When evaluating legal representation, looking at a firm’s track record is paramount. A history of successful outcomes in mesothelioma cases indicates that a firm understands the intricacies of this specific type of litigation and has the resources to pursue justice effectively. This includes having established relationships with medical and industry experts who can provide critical testimony. Furthermore, a firm with a strong reputation may find that manufacturers are more willing to settle claims, potentially leading to a faster resolution and compensation for your family. It’s about finding a team that has demonstrated its ability to achieve positive results for clients facing similar circumstances.
Client Testimonials And Recommendations
Beyond case results, hearing directly from past clients can offer valuable insights into a law firm’s approach and effectiveness. Testimonials often highlight the level of personal attention and support provided throughout the legal process. For individuals dealing with a serious illness like mesothelioma, knowing that their legal team is not only skilled but also compassionate and communicative can provide significant peace of mind. Recommendations from others who have navigated similar legal challenges can help confirm that a firm prioritizes client well-being alongside achieving justice.
Financial Considerations For Mesothelioma Claims
Pursuing a mesothelioma claim should not add to the financial strain already faced by individuals and their families. A national asbestos law firm operates on a contingency fee basis, meaning there are no upfront costs or hourly charges. This approach allows clients to focus on their health and recovery without the immediate worry of legal expenses. The firm covers the costs associated with investigating, researching, and filing the claim. Payment is only due if compensation is successfully secured on behalf of the client. This structure ensures that legal representation is accessible, regardless of a client’s current financial situation. The primary goal is to maximize the compensation recovered, not to burden the client with additional expenses.
No Upfront Costs Or Hourly Fees
Clients will not incur any charges to begin their case. The law firm assumes all financial responsibility for the expenses involved in building and submitting the claim. This includes costs for gathering evidence, consulting with experts, and filing the necessary legal documents. This financial arrangement is designed to remove barriers to justice, making legal recourse available to everyone affected by asbestos-related illnesses.
Contingency Fee Agreements Explained
A contingency fee agreement means the law firm’s payment is contingent upon winning the case. If a settlement or verdict is obtained, the firm receives a predetermined percentage of that amount. This percentage is agreed upon at the outset of the representation. If the case is unsuccessful, the client owes no attorney fees. This system aligns the firm’s interests with those of the client, as both parties are motivated by achieving a favorable outcome. Those wanting to speak with a firm directly before committing can also reach out to experienced asbestos litigation attorneys to discuss their case in a no-obligation consultation.
Maximizing Compensation From All Sources
National asbestos law firms are equipped to explore every potential avenue for compensation. This includes pursuing claims against liable manufacturers, seeking benefits from asbestos bankruptcy trust funds, and assisting with workers’ compensation claims if applicable. Their broad experience allows them to identify all responsible parties and available resources, aiming to secure the maximum possible financial recovery for the client’s medical expenses, lost wages, and other damages.

Beyond Progression: How Stem Cell Therapy in India Offers a New Horizon for Retinitis Pigmentosa Patients
Retinitis Pigmentosa is a difficult diagnosis. It is a serious genetic eye disorder. This condition causes progressive vision loss. Early symptoms include poor night vision. Tunnel vision often develops later. Conventional treatments are very limited. They mostly aim to slow the disease. Stem cell therapy now offers real hope. India is a global leader. This is a new medical frontier.
Understanding Retinitis Pigmentosa’s Challenge
Retinitis Pigmentosa is a disease group. These diseases affect the retina. The retina is light-sensitive eye tissue. It lines the back of the eye. RP destroys important photoreceptor cells. Rods and cones are these photoreceptors. Rods handle low-light vision. Cones manage detail and color vision. A genetic flaw causes this cell death. The damage is unfortunately permanent. Patients experience a slow loss of sight. This journey can feel very isolating. Daily activities become huge challenges. A person’s independence is greatly reduced. The world slowly fades away. Choosing proper Stem Cell Thearpy in India can be a proper healing option here.
The Promise of Stem Cell Therapy
Stem cells are the body’s master cells. They are unique and unspecialized. They can transform into many cell types. This ability is called differentiation. Stem cell therapy harnesses this power. Its primary goal is tissue repair. It also aims for cell regeneration. For RP the focus is the retina. Stem cells might replace lost photoreceptors. They could also protect healthy retinal cells. This offers a dual-action approach. This method goes beyond slowing the disease. It seeks to restore some lost function. This potential is truly revolutionary.
India’s Pioneering Role in Treatment
India has become a prominent hub. This hub is for medical innovation. Stem cell research is a key focus. Top Indian clinics offer modern treatments. These clinics employ expert medical specialists. They operate in state-of-the-art facilities. The treatment protocols are carefully designed. Patient safety is the highest priority. Many international patients travel to India. They seek excellent care at affordable costs. India’s regulatory environment supports this research. This atmosphere fosters ongoing breakthroughs. The nation offers significant hope. This Stem Cell Treatment for Retinitis Pigmentosa In India access changes many lives.
Conclusion
Retinitis Pigmentosa is a devastating condition. It progressively steals a person’s sight. It also takes away their independence. Past treatments offered very little solace. Stem cell therapy from India changes things. This is not about slowing the disease. It is about potential vision improvement. India makes this advanced hope accessible. The care is high-quality and available. For patients everywhere this is important. A new horizon of possibility opens. It offers a real light in darkness. Hope is now a tangible thing. This gives patients a new beginning.

PTSD and Its Impact on Mental Health
Defining Post-Traumatic Stress Disorder
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after someone experiences or witnesses a traumatic event. These events might include combat, natural disasters, accidents, or personal assaults. PTSD isn’t just about remembering the event—it’s about how the brain and body respond to it long after it’s over. For many, the trauma rewires how they perceive safety, trust, and even their own emotions.
Common Symptoms of PTSD
PTSD symptoms can vary widely, but they generally fall into four main categories:
- Intrusive memories: These can include flashbacks, nightmares, or unwanted thoughts that bring the traumatic event back vividly.
- Avoidance behaviors: People might avoid places, conversations, or even thoughts that remind them of the trauma.
- Negative changes in mood or thinking: This could mean feelings of hopelessness, difficulty remembering aspects of the event, or an overall sense of detachment from others.
- Heightened arousal or reactivity: Symptoms like irritability, being easily startled, or having trouble sleeping are common.
These symptoms can lead to considerable distress, affecting daily routines and relationships.
The Psychological and Physical Effects of PTSD
The impact of PTSD goes beyond emotional struggles. Psychologically, individuals may grapple with trust, intimacy, and communication challenges, which can strain relationships and make social interactions difficult. These difficulties often affect how survivors connect with others and solve problems in everyday life.
Physically, PTSD can manifest as chronic stress, headaches, or digestive issues. Over time, the body’s constant “fight or flight” response can even contribute to long-term health problems like heart disease or high blood pressure. Understanding these effects is key to addressing the full scope of PTSD’s impact on mental health.
The Role of Trauma Therapy in PTSD Recovery
How Trauma Therapy Addresses PTSD Symptoms
Trauma therapy is a focused approach to help individuals manage and reduce the distressing effects of PTSD. It provides a structured way to process traumatic memories, which can often feel overwhelming or impossible to face alone. By addressing the root causes of PTSD, therapy can significantly reduce symptoms like flashbacks, anxiety, and depression. Techniques such as cognitive restructuring, exposure therapy, and mindfulness exercises are often used to help individuals regain control over their thoughts and emotions. Over time, this process can lead to improved daily functioning and a sense of stability.
The Importance of Early Intervention
Getting help as soon as PTSD symptoms appear is vital. Early intervention can prevent symptoms from becoming more severe or deeply ingrained. It also allows individuals to start building coping strategies sooner, which can make the recovery process smoother. Key signs to look for include persistent nightmares, avoiding certain places or situations, and feeling constantly on edge. Recognizing these symptoms early and seeking professional support can make a significant difference in recovery outcomes. Understanding the stages of PTSD recovery highlights how early action can enhance both treatment and coping strategies.
Long-Term Benefits of Trauma Therapy
The impact of trauma therapy often extends far beyond symptom relief. It can help individuals build resilience, improve relationships, and develop a stronger sense of self-worth. Over time, therapy fosters personal growth by teaching skills that can be applied to future challenges. Additionally, the tools learned during therapy can help prevent relapses and support long-term mental well-being. For many, the journey through trauma therapy becomes a foundation for a healthier, more fulfilling life.
Types of Trauma Therapy for PTSD
Cognitive Behavioral Therapy for Trauma
Cognitive Behavioral Therapy (CBT) is one of the most widely used approaches for treating PTSD. It focuses on identifying and changing negative thought patterns that contribute to distress. Therapists often use techniques like cognitive restructuring to help patients challenge harmful beliefs and replace them with healthier ones. CBT has been shown to significantly reduce PTSD symptoms, making it a cornerstone in trauma-focused care. Sessions may also include gradual exposure to traumatic memories in a controlled setting, which helps desensitize individuals to triggers over time.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is a specialized therapy that uses guided eye movements to help reprocess traumatic memories. The idea is that moving the eyes in a specific pattern while recalling distressing events can reduce their emotional impact. This method is particularly effective for those who struggle to talk about their trauma because it doesn’t rely heavily on verbal expression. Many individuals report feeling a sense of relief and closure after completing EMDR sessions, as it helps “unstick” memories that feel frozen in time.
Somatic Experiencing and Its Benefits
Somatic Experiencing focuses on the physical sensations associated with trauma. The therapy aims to release tension stored in the body, which often manifests as chronic pain or other physical symptoms. By paying attention to bodily sensations and learning to regulate them, individuals can achieve a sense of safety and grounding. This approach is especially helpful for those whose trauma has left them feeling disconnected from their own bodies. Techniques may include breathing exercises, gentle movement, and mindfulness practices. For individuals interested in creative methods, expressive arts therapy can complement somatic work by offering a way to process emotions through art, music, or movement.
The Science Behind Trauma Therapy
How Trauma Affects the Brain
Trauma significantly alters how the brain operates, particularly in areas responsible for emotional processing, memory, and the perception of threats. For example, the amygdala, often called the brain’s alarm system, becomes hyperactive in individuals with PTSD. At the same time, the prefrontal cortex, which helps regulate emotions, may become less active. This imbalance can lead to a heightened sense of fear and difficulty distinguishing between real and perceived threats. Trauma significantly changes brain function, which explains why many people with PTSD experience persistent distress and fear long after the traumatic event has passed.
Neuroplasticity and PTSD Recovery
The brain’s ability to adapt, known as neuroplasticity, plays a vital role in recovering from trauma. While trauma can create negative patterns in the brain, therapy helps to “rewire” these pathways. Techniques like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) encourage the brain to form new, healthier connections. This process not only reduces symptoms but also helps individuals regain a sense of control over their thoughts and emotions. Understanding the brain’s capacity for change is key to effective PTSD treatment.
The Role of Stress Hormones in Trauma
Trauma impacts the body’s stress response, often leading to an overproduction of hormones like cortisol and adrenaline. While these hormones are essential for survival, their prolonged elevation can harm both the brain and body. For instance, chronic stress can shrink the hippocampus, the area of the brain responsible for memory and learning. Trauma therapy aims to regulate this hormonal imbalance, helping individuals manage their stress more effectively over time. By reducing the body’s “fight or flight” response, therapy creates a calmer internal environment, making recovery possible.
Choosing the Right Trauma Therapist
Qualities to Look for in a Trauma Therapist
Choosing a therapist for trauma therapy is a personal decision, but there are key qualities that can guide the selection process. Experience in trauma-focused therapies like Cognitive Behavioral Therapy (CBT) or Eye Movement Desensitization and Reprocessing (EMDR) is often a priority. A therapist who specializes in trauma will understand the unique challenges faced by individuals with PTSD. Additionally, empathy, patience, and strong communication skills are essential traits. Feeling comfortable and safe during sessions is just as important as their professional qualifications.
Questions to Ask During the Initial Consultation
The first consultation is an opportunity to evaluate if the therapist is the right fit. Here are some questions to consider asking:
- What is your experience in treating PTSD and trauma-related conditions?
- Which trauma therapies do you specialize in, and how do they work?
- How do you approach building trust and creating a safe environment for your clients?
The answers to these questions can provide insight into their methods and whether their approach aligns with your needs. Don’t hesitate to ask about logistics like session length, fees, and availability as well.
The Importance of Therapist-Patient Compatibility
Therapist-patient compatibility can significantly impact the success of trauma therapy. Building trust takes time, but an initial sense of connection can make the process smoother. Compatibility goes beyond shared interests; it’s about feeling understood and respected. If the relationship doesn’t feel right after a few sessions, it’s okay to explore other options. Finding the right therapist is a step toward calming the nervous system and integrating traumatic memories, which are key goals of trauma therapies.
The Process of Trauma Therapy
What to Expect in Your First Session
Starting trauma therapy can feel overwhelming, but the first session is usually about building trust and understanding your needs. The therapist will likely ask about your history, symptoms, and goals for recovery. This initial meeting sets the foundation for a tailored treatment plan. It’s also a chance to ask questions and see if the therapist feels like the right fit for you. Don’t worry about diving into deep issues right away; the focus is on creating a safe space.
Setting Goals for PTSD Recovery
Recovery goals in trauma therapy often revolve around reducing symptoms, improving daily functioning, and processing traumatic memories. These goals are typically set collaboratively between the therapist and the patient. They might include:
- Learning to manage triggers and emotional responses.
- Reclaiming a sense of normalcy in daily life.
- Building coping strategies for ongoing challenges.
Goals may evolve over time, reflecting progress or new insights gained during the therapy process.
The Stages of Trauma Therapy
Trauma therapy usually unfolds in stages, each designed to address different aspects of recovery. While every individual’s journey is unique, these are the common phases:
- Stabilization: This stage focuses on creating a sense of safety and teaching skills to handle distress, such as grounding techniques or mindfulness.
- Processing the Trauma: Here, individuals work through traumatic memories, often using methods like an evidence-based therapy for PTSD to confront and process these experiences.
- Reintegration: The final stage involves applying what’s been learned to daily life, fostering resilience, and moving forward with greater emotional stability.
Trauma therapy, also known as trauma-focused therapy, is a journey that requires patience and commitment. Each step, from the first session to the final stage, plays a critical role in helping individuals regain control over their lives.
Challenges in Trauma Therapy and How to Overcome Them
Dealing with Emotional Triggers During Therapy
One of the toughest parts of trauma therapy is managing emotional triggers. When discussing past events, emotions like fear, anger, or sadness can resurface unexpectedly. This can make therapy feel overwhelming at times. Therapists often use grounding techniques, like focusing on the present moment, to help clients regain control. Breathing exercises and mindfulness practices are also common tools for managing these intense feelings. For example, effective therapies for trauma and PTSD often incorporate mindfulness to help clients stay anchored during sessions.
Overcoming Resistance to Treatment
Resistance is another hurdle many face in trauma therapy. It’s not uncommon for individuals to feel hesitant about opening up or even skeptical about whether therapy can help. This resistance can stem from fear of reliving painful memories or a lack of trust in the process. Therapists work to build a safe and supportive environment, which helps clients feel more comfortable over time. Techniques like motivational interviewing can also encourage individuals to engage more fully in their treatment. Tailored approaches, such as effective treatments for PTSD, can make a significant difference in addressing these barriers.
Building Resilience Through Therapy
Building resilience is a long-term goal but can feel like an uphill battle, especially in the early stages of therapy. Resilience isn’t just about “bouncing back”—it’s about developing the tools to manage stress and adapt to challenges. Therapists often focus on helping clients identify their strengths and build coping strategies. Some common methods include:
- Practicing self-compassion to counter feelings of guilt or shame.
- Setting small, achievable goals to create a sense of progress.
- Engaging in activities that promote emotional well-being, like journaling or creative arts.
Over time, these steps help individuals feel more empowered to navigate life’s challenges, making the therapy process more rewarding.
The Role of Support Systems in PTSD Recovery
How Family and Friends Can Help
When someone is dealing with PTSD, the support of family and friends can make a world of difference. Loved ones play a critical role in creating a safe and understanding environment where the individual feels heard and accepted. Simple actions, like being patient and listening without judgment, can go a long way. Offering to help with daily tasks or just being present during tough moments also provides a sense of stability. It’s important for family members and friends to educate themselves about PTSD so they can better understand what their loved one is going through.
The Importance of Support Groups
Support groups are another vital resource for individuals recovering from PTSD. These groups provide a space where people can share their experiences and connect with others who truly understand what they’re going through. For instance, peer support is crucial for individuals with PTSD, as it fosters acceptance and alleviates feelings of isolation. In these groups, participants often find comfort in knowing they’re not alone, which can be incredibly empowering. For returning war veterans, peer support groups are especially beneficial, helping them rebuild social connections and reduce PTSD symptoms. Joining a support group can be a stepping stone toward healing and building resilience.
Integrating Community Resources into Recovery
Community resources can also play a significant role in PTSD recovery. Local organizations, mental health centers, and even online platforms often offer programs tailored to individuals coping with trauma. These might include counseling services, workshops, or recreational activities aimed at reducing stress. Utilizing these resources can complement trauma therapy and provide additional layers of support. It’s all about creating a network of care that surrounds the individual with the tools they need to recover. Communities that prioritize mental health awareness make it easier for people to seek help without fear of judgment or stigma.
Self-Care Practices to Complement Trauma Therapy
Mindfulness Techniques for PTSD
Mindfulness is one of the most effective ways to manage PTSD symptoms. It encourages individuals to focus on the present moment, helping to reduce feelings of anxiety and distress. Simple practices like deep breathing, body scans, or guided meditations can make a big difference. For instance, spending just 10 minutes a day practicing mindfulness can help calm the mind and create a sense of control. Consistency is key—making mindfulness a daily habit can amplify its benefits over time.
The Role of Physical Activity in Recovery
Engaging in regular physical activity can improve mental health and support PTSD recovery. Exercise doesn’t have to mean running marathons or lifting heavy weights. Activities like yoga, walking, or even dancing can be beneficial. These movements not only release endorphins but also help individuals reconnect with their bodies. In fact, techniques such as myofascial release have been shown to aid in releasing trapped emotions and tension. Finding an activity that feels enjoyable and sustainable is crucial for long-term success.
The Importance of Nutrition and Sleep
Good nutrition and quality sleep are often overlooked but are vital for emotional and physical well-being. Eating a balanced diet rich in whole foods, lean proteins, and healthy fats can stabilize mood and energy levels. Similarly, establishing a consistent sleep routine can significantly improve PTSD symptoms. If sleep is a challenge, creating a calming bedtime ritual—like turning off screens an hour before bed or sipping herbal tea—can help. It’s also helpful to consult a trauma expert for personalized strategies, as healing is a gradual process (managing PTSD).
Measuring Progress in PTSD Recovery
Recognizing Signs of Improvement
Understanding progress in PTSD recovery can be tricky because it often varies from person to person. However, there are some common indicators that therapy is working. For instance, individuals might experience fewer intrusive thoughts or nightmares. They may also notice a reduction in avoidance behaviors, like being able to visit places or engage in activities they previously avoided. Emotional regulation also tends to improve, with fewer outbursts or overwhelming feelings. Improvement isn’t always linear, but recognizing these small changes can provide reassurance that recovery is happening.
The Role of Feedback in Therapy
Feedback plays a big role in measuring progress. Therapists often ask patients to share their thoughts on how therapy is going and whether they feel the sessions are helping. This kind of open communication helps in adjusting the treatment plan if needed. Self-assessment tools, like mood trackers or symptom checklists, can also be helpful. These tools give both the therapist and the individual a clearer picture of what’s working and what might need tweaking. Honest feedback is key to making therapy as effective as possible.
Adjusting Treatment Plans as Needed
No two PTSD recovery journeys are the same, which is why flexibility in treatment is so important. Sometimes, a specific therapy approach might stop being effective, or new challenges might arise that require a shift in focus. Regular evaluations help ensure the treatment plan stays aligned with the individual’s needs. This might mean incorporating new techniques, like mindfulness exercises, or revisiting earlier strategies that worked well. Adjustments aren’t setbacks—they’re part of tailoring the recovery process to best support the individual.
Addressing Stigma Around PTSD and Trauma Therapy
Breaking Down Misconceptions About PTSD
PTSD is often misunderstood, leading to widespread misconceptions. Some people wrongly believe it only affects veterans or those who have experienced extreme violence. In reality, PTSD can arise from various traumatic events, such as accidents, natural disasters, or personal losses. Educating the public about the diverse causes and symptoms of PTSD is a key step toward reducing stigma.
To break these misconceptions:
- Share real-life stories of individuals from different backgrounds who live with PTSD.
- Promote accurate information through social campaigns and educational programs.
- Encourage media outlets to portray PTSD in a realistic and compassionate manner.
Encouraging Open Conversations About Mental Health
Talking about mental health openly can feel intimidating, but it’s one of the most effective ways to challenge stigma. People often avoid these discussions out of fear of being judged or misunderstood. By normalizing these conversations, individuals can feel more comfortable seeking help and sharing their experiences.
Here are a few ways to start:
- Use “I” statements to express personal feelings and experiences, fostering understanding and empathy. Overcoming mental health stigma can begin with small, honest dialogues.
- Host community events focused on mental health awareness.
- Support friends or family members by listening without judgment and validating their feelings.
The Role of Advocacy in Reducing Stigma
Advocacy plays a powerful role in shifting public attitudes about PTSD and trauma therapy. When individuals, organizations, and communities come together to speak up, they can influence policies, improve access to care, and create a more accepting society.
Advocacy efforts might include:
- Joining or supporting mental health advocacy groups.
- Participating in events like PTSD awareness walks or fundraisers.
- Sharing personal journeys to inspire others and challenge stereotypes.
By embracing therapy and promoting self-awareness, individuals can challenge the stigma surrounding mental health. Seeking help isn’t a sign of weakness; it’s a step toward transformative life changes. Embracing therapy can empower people to reclaim their lives and find strength in their recovery.

Double Eyelid Surgery: Detailed Information
An Asian blepharoplasty is an operation to create a crease in the upper eyelid. It is done by forming the crease more accurately, making the eyes appear wider. The space between the upper and lower eyelids increases.
What Is Double Eyelid Surgery?
Most Asians have double eyelids, where the upper eyelid lacks a crease. In this kind of surgery, the surgeon makes a fold, creating a false impression of bigger eyes. This type of surgery is mainly done on Asian women who have monoids with a wish to appear more Westernized or feminine. However, there are some key factors one should consider, including what’s important, what should be done first, what risks are involved, and what other options exist.
Types Of Double Eyelid Surgery
The various types include:
- Full incision double eyelid surgery (กรีด ตา สอง ชั้น, which is the term in Thai) involves the surgeon cutting along the new eyelid crease and using removable stitches to support it while it heals. It is recommended for those with excess fat or extra skin on their upper eyelids.
- Partial incision eyelid surgery is a modification of the complete incision technique, which is associated with a smaller wound length. It is intended to minimize scarring during reshaping of the eyelid.
- No cut eyelid surgery is appropriate for people whose infraorbital skin or fat does not require an excision. The surgeon aims to form a new crease by passing strings through the eyelid with small openings. This is the most straightforward technique to reverse among them all.
Risks Of Double Eyelid Surgery
Adverse effects commonly occur are complications from eyelid surgery, including numbness, infection, and difficulty closing eyes completely, resulting in dehydrated eyes. In terms of patient satisfaction, some Asians and Asian Americans could be unhappy due to peculiarities in their eyelids that make the operation more complicated for them. The result may need improvement.
Final Thoughts!
In summary, Asian eyelid surgery (double blepharoplasty), which is a type of plastic surgery that aims to create a fold in the upper eyelid so that the eyes look bigger, is practiced by many. This can vary because there are incapacitating, partially incapacitating, or non-incapacitating ways that are possible.
Nevertheless, complications such as infection and numbness after surgery concerning various configurations of eyelid types should be kept in mind to prevent the eyelid from being unappealing. To decide whether or not you need to get eyelid surgery or even understand the procedure and potential risks, you must learn everything about it.
How Much Does a Labiaplasty Surgery Cost?
In the fields of plastic surgery and obstetrics, female genital cosmetic surgery (FGCS) is a trending surgical technique. This refers to any genital surgery meant to improve genital appearance but not medically essential. Among these operations is labiaplasty, which modifies the inner or outer lips of a woman’s genitalia in terms of size and form. To create a more symmetrical appearance, the surgeon meticulously eliminates excess tissue from the labia and restructures them throughout the treatment. Labiaplasty is a treatment for female genitalia that patients consider for medical tourism in Dubai, similar to other cosmetic surgeries like rhinoplasty, facelift, and many more.
Cost Of Labiaplasty In Dubai
In Dubai, a labiaplasty typically costs 15000 AED or 4084 dollars. The severity of the issue that has to be fixed will be one of the many elements that determine Labiaplasty cost in Dubai, UAE.
Package For Labiaplasty In Dubai
The cost of a labiaplasty in Dubai can vary based on the surgeon and the clinic. The package usually includes:
Meet with a plastic surgeon to go over your desired results and assess your suitability for the procedure.
A physical examination and blood testing are pre-operative treatments.
Anesthetic expenses.
The price of the procedure for labiaplasty.
Utilization of the operating room and surgical tools.
Post-operative treatment includes follow-up appointments with the surgeon to monitor your healing progress and address any problems.
Prescription drugs for the treatment of pain and the avoidance of infections.
Factors Impacting The Cost Of Labiaplasty In Dubai
The scope of the procedure:
The cost of a labiaplasty procedure can be affected by its complexity, which includes the amount of tissue that is removed or reshaped.
Experience and qualifications:
Highly skilled and certified plastic surgeons may command higher fees because of their reputation and level of expertise.
Location:
Depending on the clinic or hospital’s location, labiaplasty costs can change. In general, procedures carried out in larger cities or wealthier locations could cost more.
Facility fees:
The total cost of the labiaplasty surgery may vary depending on the cost of using the facility, which includes the operating room, nursing personnel, and other related expenses.
Anesthesia fees:
The price of the anesthesia used during the procedure may also affect the cost of a labiaplasty in Dubai.

Advice For Treating Acne Scars
Many people experience dissatisfaction and insecurity due to acne scars. Although it may be difficult to eliminate acne scars, several treatments come under Best Way to Cure Acne Scar (รักษารอยสิวอย่างไรดี, which is the term in Thai). The finest treatments for acne scars that will also give your skin a healthy glow are mentioned here.
Prevent Sun Damage
To avoid further damage to acne scars, you must shield the skin from the sun’s harmful rays. Even on overcast days, always use broad-spectrum sunscreen with an SPF of at least 30. Applying sunscreen before going outside can stop hyperpigmentation and keep scars from getting darker.
Localized Therapies:
Acne scars can be reduced in visibility by using topical treatments. Cell turnover, fading hyperpigmentation, and stimulating collagen formation are all possible outcomes of using ingredients like retinoids, alpha hydroxy acids (AHAs), and vitamin C. However, because of the potential for irritation or sensitivity, these therapies should only be used under the supervision of a dermatologist.
Acid Peels:
Chemical peels are an exfoliating treatment that stimulates new skin cell growth by applying a chemical solution to the skin. They improve skin texture and tone while diminishing the appearance of acne scars of mild to moderate severity. The depth of the peel must be adjusted according to the patient’s skin, thus it’s important to have a professional do the treatment.
Microneedling:
Collagen induction therapy, or micro-needling, is a treatment in which tiny needles induce controlled micro-traumas in the skin. Acne scars may gradually fade through this process because collagen production is increased. For optimal safety and effectiveness, micro-needling should be performed by an experienced medical professional.
Laser Treatment For Health Issues:
Fractional laser and intense pulsed light (IPL) are two types of laser therapy that can reach the dermal layers of the skin and trigger collagen synthesis. Acne scars can be diminished and the skin’s texture improved by these methods. However, you may need to schedule many appointments, and you must follow all post-treatment recommendations to the letter.
Lip Fillers:
Acne scars that have been depressed can be made less noticeable with the help of dermal fillers, which are injected to add volume to the skin. Hyaluronic acid fillers are frequently utilized for this purpose because of their quick effectiveness and low recovery time. The effects normally wear off after a while, and further treatments are required to keep them going.

Dental Social Security: Ensuring Your Oral Health For A Worry-Free Future
Hey there! Are you ready to dive into the world of dental social security (ทําฟัน ประกันสังคม which is the term in Thai)? We’ve got you covered! In this article, we’ll explore the importance of maintaining oral health to secure a future filled with confident smiles.
From understanding common dental issues to learning about preventive measures and available treatments, we’ll provide the information you need to keep your pearly whites in top shape. So, let’s get started!
The Foundations Of Dental Social Security
When we talk about dental social security, we’re referring to the steps you can take to safeguard your oral health and prevent potential dental problems. As you plan for retirement or set up an emergency fund, prioritizing your dental well-being can save you from costly treatments and ensure a happy, healthy smile.
Maintaining good oral hygiene is the cornerstone of dental social security. Brushing your teeth twice daily, using fluoride toothpaste, and flossing regularly is essential to keep your teeth and gums strong. Remember, prevention is key!
Common Dental Issues And Their Impact
Understanding the common dental issues that can arise is crucial for taking proactive measures to protect your oral health. Let’s take a closer look at some of these concerns:
· Tooth Decay: A Sneaky Intruder
Tooth decay, also known as cavities, occurs when bacteria in your mouth produce acids that erode tooth enamel. If left untreated, this can lead to painful toothaches, sensitivity, and even tooth loss. Regular dental check-ups and a healthy diet low in sugary foods and beverages can help keep tooth decay at bay.
· Gum Disease: Don’t Let It Sneak Up On You
Gum or periodontal disease affects the tissues that support your teeth. It begins with gum inflammation (gingivitis) and, if not addressed, can progress to more severe stages. Early signs include swollen, bleeding gums and persistent bad breath. Brushing, flossing, and routine visits to your dentist play a vital role in preventing gum disease.
· Oral Cancer: The Importance Of Early Detection
Oral cancer is a severe condition that affects various parts of the mouth, including the tongue, lips, and throat. It’s essential to be aware of any changes or abnormalities, such as lumps, sores that don’t heal, or difficulty swallowing. Regular dental check-ups include oral cancer screenings, enabling early detection and increasing the chances of successful treatment.
Conclusion
Dental sealants are thin protective coatings applied to the chewing surfaces of your back teeth. They create a barrier against bacteria and food particles, reducing the risk of cavities. This quick and painless procedure can be especially beneficial for children and teens struggling with proper brushing techniques.

Five Things You Should Know About Laparoscopic ACL Surgery
The anterior cruciate ligament (ACL) is one of the four major ligaments in the knee. An ACL tear can occur during sports activities involving sudden stops or direction changes, such as football, soccer, and basketball. If you’re unsure whether you have an ACL tear, check out this article by Ray of Health. Laparoscopic ACL surgery is a minimally invasive procedure used to repair a torn ACL.
If you are considering laparoscopic ACL surgery, you should know a few things. In this blog post, we will discuss five things you should know about Laparoscopic anterior cruciate ligament surgery (ผ่าตัด เอ็นไขว้หน้าแบบส่องกล้อง, which is the term in Thai)
1. What Is Laparoscopic ACL Surgery?
Laparoscopic ACL surgery is a minimally invasive procedure used to repair a torn ACL. It is performed through several small incisions in the knee. A camera is inserted through one of the incisions, and the surgeon uses the camera to view the inside of the knee. The surgeon then inserts surgical instruments through the other incisions to repair the ACL.
2. Who Is A Good Candidate For Laparoscopic ACL Surgery?
It is a good option for people with torn ACL, are active, and want to return to their previous activity level. It is also a good option for people with other medical conditions that make traditional ACL surgery more risky.
3. What Are The Risks Of Laparoscopic ACL Surgery?
The risks are similar to those of traditional ACL surgery. These risks include infection, blood clots, and nerve damage. However, the risks of laparoscopic ACL surgery are generally lower than the risks of traditional ACL surgery.
4. What Is The Recovery Time For Laparoscopic ACL Surgery?
The recovery time is generally shorter than that for traditional ACL surgery. Most people can walk without crutches within a few days of surgery. They may need to use a brace for several weeks. Full recovery can take up to six months.
5. What Are The Benefits Of Laparoscopic ACL Surgery?
The benefits of laparoscopic ACL surgery include a shorter recovery time, a lower risk of infection, and a smaller scar. It can also be performed on people with other medical conditions that make traditional ACL surgery more risky.
Conclusion
Laparoscopic ACL surgery is a minimally invasive procedure used to repair a torn ACL. It is a good option for active people who want to return to their previous level of activity. It is also a good option for people with other medical conditions that make traditional ACL surgery more risky.
If you are considering laparoscopic ACL surgery, talk to your doctor about the risks and benefits of the procedure.
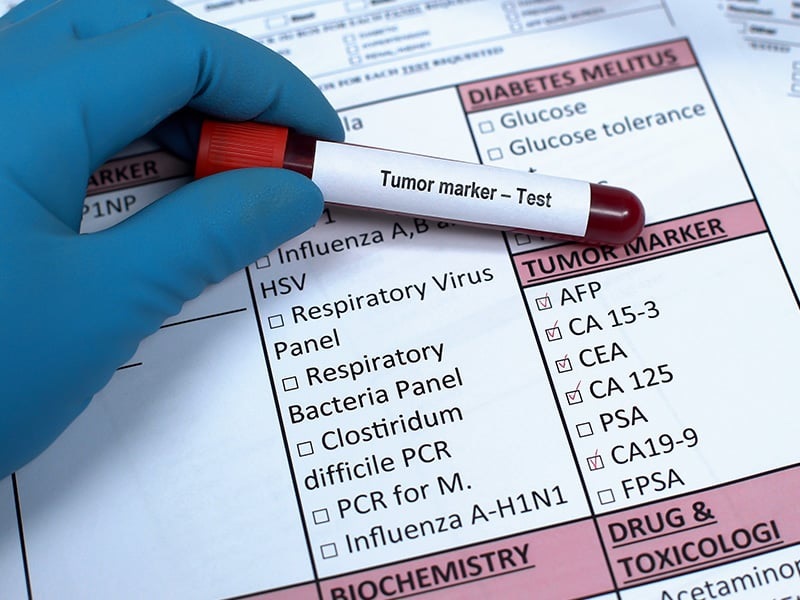
What are tumor markers in blood test?
Health is always a thing that is taken for granted. People will only appreciate the gift of health when they actually experience some form of disease or sickness. There are many forms of health problems that affect people of all ages. One of the terrifying forms of disease affecting health greatly is cancer. It is so terrifying that even mentioning the word ‘cancer’ can send shivers down the spine in a split second. There are more than 100 types of cancer that have been identified. 50{a2a46ec55642e682a71e8cca36f3803ecd4bd950ef2bece5716193f567526501} of all cancer cases are actually preventable which means regular health screening should be able to detect it at its early stage. In this article, we will be learning about tumour markers in blood tests that are associated with cancer diagnosis.
Tumour marker is a substance produced by the body as a response to cancer or certain benign conditions. It has traditionally been proteins or other substances that are produced in higher amounts by the cancer cells than the normal cells. In general, tumour markers can be found in the blood, urine, stool, tumour and other tissue or body fluids of a person with cancer. Tumour markers are also known as biomarkers. Some of these tumour markers are specific to one cancer whereas some may be seen in several types of cancer. Testing for tumour markers in blood tests is usually performed by taking a sample of blood to be analysed in the laboratories.
There are two main types of tumour markers: tumour tissue markers and circulating tumour markers. Tumour tissue or cell markers are found in the tumour, typically in a sample of tumour obtained from biopsy. Circulating tumour markers are found in blood, urine, stool or other body fluids. Hence, tumour markers in blood test are classified as circulating tumour markers.
It is true that high tumour marker levels can be a sign of cancer. Tumour marker tests, specifically circulating tumour marker is used for several reasons such as to estimate the prognosis or outcome of the cancer, to determine the stage of cancer, to identify remaining cancer cells after treatment, to identify if the cancer cells have returned after treatment (recurrence), to assess treatment progress and as a monitor to know if a treatment has stopped working or ineffective.
In reality, circulating tumour markers are not enough to diagnose cancer although elevated levels of this marker may suggest a person with cancer. This is because even noncancerous conditions may lead to an increase of certain tumour markers. Plus, people with a particular type of cancer may not have a higher level of tumour marker to be suspicious with the specific cancer. Some cancers do not produce tumour markers that can be found in the blood test. Thus, circulating tumour markers are usually combined with other results such as from biopsy or imaging test to diagnose cancer.
Example of commonly used tumour marker in blood test includes:
1) Calcitonin- One of the hormones produced by thyroid but increased of calcitonin level is associated with medullary thyroid cancer. Calcitonin biomarkers are most often used to diagnose medullary thyroid cancer, to know if treatment for the cancer is working, to check for recurrence possibility and to estimate prognosis.
2) CA 125- Ovarian cancer is the most common cause for elevation of this biomarker but cancers of the uterus, cervix, breast, lung, liver, pancreas, colon and digestive tract may also raise the level. CA 125 is mainly used to monitor how well treatments for ovarian cancer.
3) Beta-2 microglobulin- Increased amount of this biomarker in blood could indicate cancer such as multiple myeloma and lymphoma.
4) Alpha-fetoprotein (AFP)- Elevated level of AFP may indicate liver cancer or cancer of ovary/testicle.
5) Beta-human chorionic gonadotropin (Beta-hCG)- May indicate cancer in testis, ovary, liver, stomach, pancreas and lung.
6) Carcinoembryonic antigen (CEA)- Colorectal cancer is the most common cancer that elevates this tumour marker.
7) Prostate-specific antigen (PSA)- High level of PSA level may indicate prostate cancer but noncancerous conditions such as benign prostatic hyperplasia (BPH) and prostatitis may increase PSA.
It can be concluded that tumour markers play many roles in cancer. From identifying cancer to the ability to assess the outcome of the cancer, tumour markers make it possible. There are a wide range of tumour markers used to describe the many ranges of cancer types. Commonly used tumour markers as mentioned above are just the small portion of tumour markers available.
Since tumour markers can be used to predict response of a cancer treatment and for prognosis, researchers hoped that tumour markers could be used as screening tests to detect cancer early on, even before symptoms are exhibited. This can be a great advantage in better management of cancer and can potentially be a means of prevention.
However, for now, tumour markers may not be suitable for cancer screening due to the low specificity and low sensitivity in detecting cancer. Fret not, many current researches have highlighted other ways to help early cancer detection, providing better effective treatment and to improve accuracy of predicting chance for cancer outcome along with its possible recurrence. It is hoped that in the near future, cancer diseases can be managed well and hopefully lessen patient’s sufferings.

Importance Of Determine Your Facial Shape
Understanding all about face shape and determining the same can help you to pick the right makeup and haircut. That said, there are six standard face shapes including square, round, rectangle, oval, heart, and diamond.
Is It Important To Determine Your Face Shape?
Knowing your face shape can help you to experiment with dimension.
· Precise Sculpting
Once you understand all about face shape, you can know the best techniques for sculpting and contouring your face. Considering the nuances of facial shape is key to applying the contour like a pro. It doesn’t matter whether you have a diamond face shape or a square one. On knowing the shape, you can work toward the center of your face and around the perimeters as well for a flawless look.
· Emphasis On The Right Feature
Once you are confident about your face shape, you can learn which part of your face needs more emphasis. This way you can focus more on that facial feature and help your face to shine and look attractive. For example, if you are round-faced, then you can consider applying the blush higher up on the cheekbones and emphasize your bone structure.
· Deemphasize The Right Facial Part
Understanding all about face shape (โครง หน้า ต่างๆ, which is the term in Thai) can help you to deemphasize better. In case you are blessed with a square jawline, you can rely on contouring makeup to achieve roundness and softer edges.
· Perfect Haircut
Your hairstyle plays a pivotal role in making and breaking your look. The right one will also emphasize your face. If you are facing difficulties in choosing the right haircut, then learning all about your face shape might come of great help. Knowing all about face shape can help you determine the right hairstyle based on your feature.
Are Considering Facial Features Important To Determine Face Shapes?
Apart from face shape measurement, there are various characteristics attached to particular face shapes. For example, a rounded jawline is synonymous with rounder faces, while a pointer chin is more associated with a heart face. Consider the contours and angles of your face to check if they are defined, sharp, or soft. Now once you have every measurement, sort out from the list of face shapes to check which one is yours.
Remember not everyone can be categorized under a singular facial shape. Many people have a combination of two or more face shapes. If none of the measurements align with a particular category, then fret not, as you aren’t alone in this. Mixtures of various facial shape is completely possible.












